Government Policy Forces Insurance Providers To Pay for Ineffective Addiction Treatment
While People Drown in the Hands of Addiction Treatment
How Health Insurance are Throwing Money Away and Hurting Enrollees In the Process
Health insurance providers have been increasingly under fire for the rising costs of premiums and costs of healthcare in general. Since 2008’s Mental Health Parity and Addiction Equity Act (MHPAEA) and 2010’s Patient Protection and Affordable Care Act (PPACA) mandated coverage of substance use treatment and services by health insurers and group health plans on par with the insurance coverage provided for medical and surgical needs, the cost and complexity of providing effective, efficient services for substance use while maintaining a strong economic presence in the market has become increasingly difficult (O, 2014). That situation is unlikely to ease unless health insurance providers consider expanding their coverage to more efficient, effective models for addiction help.
National Costs of Substance Use
Substance abuse in the US costs $600 billion dollars annually. The recent Surgeon General’s report on addiction (2016) notes that, in a 2015 survey, 27 million people reported using illicit drugs or misusing prescription drugs and 66 million reported at least one episode of binge drinking within the last 30 days. This substance use translated into an annual cost to the US of $193 billion for illicit drug use and $249 billion for alcohol use with $120 billion dollars of that in healthcare costs. Substance Use Disorder (SUD) is estimated to affect 20.8 million Americans or 8% of the adult and adolescent populations. If you count in the family members affected by someone with a SUD, the numbers become 1 in 3 people affected so everyone knows someone or has been affected by substance use, directly or indirectly.
Direct Versus Indirect Costs
Substance use has both direct and indirect costs. Direct costs are costs such as healthcare and addiction treatment costs. Indirect costs are ancillary costs as a result of substance use, including economic costs due to absenteeism, loss of productivity, or disability; personal and community losses due to premature death or impairment, or crimes related to substance use and the criminal justice cost of prosecution and incarceration (Trautmann, 2016).
While indirect costs of substance use are significantly higher than the direct costs (indirect costs are estimated to run just over $442 billion annually), we will focus on healthcare costs and not costs of incarceration, economic losses, etc.
Are Addiction Research Dollars Being Well Spent?
As a nation, we spend billions annually on healthcare research and treatment in an attempt to lessen the effects and even eliminate illness and disease. When it comes to healthcare dollars for research and care spent on SUD versus chronic illnesses, it becomes clear quickly that there are important differences in the results of both research and healthcare dollars spent.
For research into chronic diseases, the US is a leader in innovative health discoveries and our research programs are well supported and funded. Investments in research to treat cancer, stroke, and heart disease have all yielded significant advances in overall lives saved, increased quality of life for patients, and new treatments to reduce or eliminate the disease effects.
Unfortunately, substance use research has not attained similar results. Moving forward with either disease or brain based models of substance use have not produced significant increases in lives saved, increased quality of life for substance users, or new treatments that reduce the effects or “cure” addiction. In fact, the numbers, effects, and expenses of overdoses are climbing and more people are meeting the criteria for SUD and AUD. The addiction research using medical models isn’t yielding results that put us in a better place as individuals or as a society.
2008 – 2012 Drug Addiction Research (Source: http://www.soberforever.net/addictionblog/index.php/how-to-waste-1-6-billion-dollars-a-year/ )

2008 – 2012 Outcome from Drug Addiction Research.
Overdoses Leading Cause of Death for Americans 50 and Younger
When it comes to the use of healthcare dollars in substance use, the direct healthcare costs are estimated to be $120 billion dollars annually (Surgeon General, 2016). There are additional costs in dealing with addiction, some of which may not be obvious.
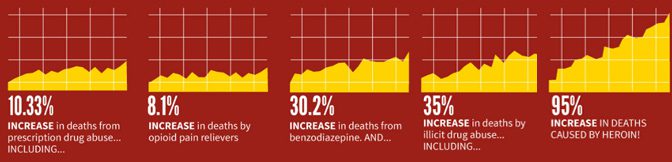
Overdoses are increasing at an alarming rate and we probably don’t yet know the true extent. In 2017, the CDC announced that, for the first time in 50 years, the life expectancy rate fell for a second year in a row (Thielking, 2017). Of the 5 leading causes of death nationally, the most significant change was seen in unintentional injuries which rose to number 3, a cause of death which had always lagged behind chronic lower respiratory disease, the former third place holder for cause of death.
Overdoses are reported under the unintentional injuries category and 2016 saw 63,600 overdoses recorded nationally. The fastest growing age group for overdoses was 25-54 and predominantly affected males.
Overdose rates has curbed their growth from 2006-2014 at a rate of 3% per year when previously, from 1999-2006, the overdose rate grew 10%. 2014-2016 saw overdose rates explode at a growth rate of 18%, which correlates with the rising use of synthetic opioids and analogs in the illicit drug culture.
- Overdose Rate 1999 – 2006 10%
- Overdose Rate 2006 – 2014 3%
- Overdose Rate 2014 – 2016 18%
Overdose Costs and Complications Rise As Synthetic Opioids Flood the Market
While more overdose patients are arriving alive at the hospital, they tend to be in worse shape and needing extensive treatment, including ICU level care and extended after care due to permanent injuries and effects. The response by communities, advocates, and legislators to increase access and training for the opioid reversal drug Narcan has helped save lives and increase the chances that a person will survive to receive medical attention. Unfortunately, survival comes at the costs of increased injury and medical resources needed to treat overdose patients in the ER/ED, ICU, and aftercare, especially with synthetic opioids and analogs appearing more frequently in the illicit drug supply.
According to a study done in 2016 covering 4.1 million patients admitted to 162 ICUs in 44 states, opioid-related overdoses accounted for just under 22,000 of those admissions (Stevens et al., 2016). The death rate rose more than 2.5% for overdose patients admitted to the ICU .
Overall, opioid overdose deaths have also doubled since 2000. ICU admissions for these overdoses rose 34% from 2009-2015 and average ICU costs for these admissions rose from $58,800 to over $92,000 in the same period.
Long-term complications of drug overdoses are increasing in frequency with the growing synthetic opioid use and include treatment for aspiration pneumonia, rhabdomylosis, brain damage, septic shock, organ failure, need for mechanical ventilation, and dialysis. Any of these complications can significantly add to the increasing cost of ICU care for opioid overdoses and some costs can extend well beyond the hospitalization, if there are permanent injuries. For example, hemodialysis for one patient costs approximately $89,000 annually or $42 billion nationally, with $34 billion of that cost is paid by Medicare (UCSF Kidney Project, 2013).
If a kidney transplant is available and approved, the cost of transplant surgery is around $32,000 with an additional annual cost of $25,000 per year per patient for post-surgical care and medications to reduce the chance of organ rejection and failure.
Drug-Related Healthcare Costs Have Far Reaching Effects
The direct costs don’t stop there unfortunately. Prior to the upsurge of synthetic opioids and analogs into the illicit drug supply, the US was already paying enormous costs for drug-related healthcare needs. Illicit drug use often comes with increased needs for treatment of Hepatitis B and C; HIV, tuberculosis, and neonatal abstinence syndrome (NAS), among other drug use related diseases and complications.
The lifetime cost of HIV treatment for one patient in 2010 dollars is estimated at $379,668 alone (CDC, 2017). The treatment for a single patient with NAS can cost $68,856, not including the lifetime costs for any medical and/or clinical services and treatments required due to permanent impairments (Jiang et al., 2017).
In 2011, the US Department of Justice’s National Drug Intelligence Center took a look at how illicit drugs impact the US economy. At that time, costs of treatment of illicit drug use annually in hospitals and ER/EDs was over $3.3 billion dollars. Additionally, treatment of diseases acquired as a result of illicit drug use included annual costs for HIV treatment at over $512 million, Hepatitis B treatment at nearly $10 million, Hepatitis C at almost $34 million, tuberculosis at just over $14 million, and an “Other” catchall category that accounted for $1.7 billion in treatment dollars. Treatment costs for illicit drug induced homicides at the nation’s hospitals and ER/EDs for the same period were almost $13 million dollars annually.
The Cost of Treatment Times 3
Per patient, the cost of addiction treatment is no less shocking and also rising. For many people, addiction treatment is not a one-time trip to end a problem for good so the costs multiply quickly over time. Often the stays and treatment costs escalate as individuals fail treatment repeatedly and more intensive treatments and services are utilized.
The average heroin use disorder (HUD) was treated at a cost of $9,187 per episode in 2011 dollars with the average patient attempting treatment 3 times (Mccollister et al., 2009).
By 2015, the average cost of a residential stay for treatment was $33,424 with detox being an additional $104,418. If the numbers hold true and each patient attempts treatment 3 times, the total healthcare costs for a heroin user just for detox and a residential stay 3 times over is slightly more than $414,500 and no guarantee that the addiction will end or that the treatment bills will cease.
%
INCREASED COST IN TREATING A HEROIN USER IN THE LAST 4 YEARS
Substance Users- Small Group of Healthcare Super Utilizers
Further evidence that substance users are super utilizers of health care dollars comes from information on the societal cost of certain diseases (Jiang, et al., 2017) . COPD (chronic obstructive pulmonary disease) cost an average of $2,567 in 2015 healthcare dollars to manage. It’s estimated that there are15 million patients with COPD for a national cost of $38.5 billion annually.
Diabetes costs the average patient $11,148 to manage annually and affects an estimated 22.3 million patients with a total cost in 2015 healthcare dollars of $248.59 billion. Both these diseases have continued to rein in costs and increase life expectancy and quality with continued research and treatment. Heroin use disorder (HUD) cost an average of $50,799 in 2015 to deal with and affected just over 1 million users at a societal cost of $51.2 billion. A typical heroin user is using almost 5 times the healthcare dollars of the typical diabetic patient and 25 times the healthcare dollars of someone with COPD while carrying the added risk of needing treatment for various drug use related diseases (Hepatitis, HIV, etc) and significant complications due to organ failure or dialysis needs, among others.
MHPAEA not only required increased access to treatment and coverage of addiction treatment but it mandated equity and parity of that coverage with the medical /surgical system coverage in place (SAMHSA, 2014). Insurance providers had to provide access and coverage with equal rates, timing of that access process, and similar systems of determining what was covered. In the past, some insurance providers who did cover behavioral health and/or addiction treatment had made access so difficult and timing of access so long that it was not feasible to use insurance and the rate covered was not comparable to a medical/surgical need. While PPACA and MHPAEA mandated access and coverage, there were gaping holes as to how this system would function. The “easiest” solution was to borrow the system employed by medical/surgical claims and shoehorn behavioral health and addiction treatment into it. The results have been less than stellar and health policy advocates think they know why.
Diabetes Cost Per Patient in Dollars
Heroin Use Cost Per Patient in Dollars
That Is Almost 500% MORE
The Demand for Parity from a Flawed System
Dr. Monique Yohanan, senior physician editor at MCG, and Richard Frank, currently a professor of health care policy at Harvard Medical School and former assistant secretary of planning and evaluation at DHHS under the Obama administration, agree that parity in behavioral health and addiction treatment is still lacking and is likely to remain so as there aren’t quick fixes for the systemic issues at fault (Kirkner, 2018). Lingering issues implementing MHPAEA arise from trying to work with addiction treatment coverage in a health insurance framework based on medical and surgical constructs.
The challenges include the lack of objective testing available for diagnosis and treatment recommendations and how to implement non-qualitative treatment limitations (NQTLs) for use in addiction treatment coverage. (For an overview of how MHPAEA and ACA work for health insurance coverage of addiction, please see http://www.baldwinresearch.com/addiction-treatment-insurance-coverage.cfm )
How Objective Can We Be? Not Very…
The medical framework of health insurance is built on objective test results to support the presence and severity of a problem and help determine the appropriate level of intervention, which can be further described through medical coding systems of International Classification of Diseases (ICD) and Current Procedural Terminology (CPT). These coding systems then allow for a requisite reimbursement rate from insurance when the criteria is met.
Dr. Yohanan, in her white paper (2017), uses the example of diagnosing diabetes and determining the level of intervention with blood tests and other objective criteria. Objective tests just don’t exist for issues like substance use. The lack of objective testing poses an added problem in trying to demonstrate parity of health insurance coverage has been achieved between medical/surgical coverage and behavioral health/addiction coverage.
One of the most widely used types of diagnostic and intervention models for addiction treatment are the criteria developed and advocated by American Society of Addiction Medicine (ASAM ), but, they too, rely heavily on subjective measures (ASAM, 2018). ASAM criteria is currently required in 30 states and utilized by many health insurance providers. It consists of 6 dimensions with 5 levels of care to create “a holistic, biopsychosocial assessment” of an individual in order to develop service and treatment planning and determine appropriate levels of care. After training, professionals can use a computer-guided interview program called Continuum to help with decision-making but it remains a completely subjective process.
Can Parity Truly Be Achieved in a Quasi-Medical Framework?
Implementation of NTQLs for addiction treatment coverage is an inexact and laborious process, both to construct and administer, to ensure parity of coverage of addiction treatment. Again, the NTQLs taken from the medical system framework don’t translate as well to a system seeking to cover behavioral health issues and substance use.
The medical disease process has tests to obtain values, definable parameters of diagnosis and severity, and can fairly efficiently determine changes that indicate a need for increased intervention and speed in decision-making to prevent further harm. NTQLs can be frustrating and difficult enough to administer in a medical/surgical system but the added burden of avoiding “warning signs” of violation of the MHPAEA and cries of discrimination in the substance use arena makes the process fraught with perils and possible expensive missteps for insurance providers.
As NAMI (National Association on Mental Illness) and other advocacy groups move to bring forth issues of systemic discrimination as a way to ensure national parity standards of behavioral health and substance use treatment coverage are met, it can feel for health insurers that they’re damned if they do and damned if they don’t.
Determining Addiction Treatment Coverage When Accountability Is Lacking
Insurance companies are at a disadvantage to determine the effectiveness of a treatment provider as the failure is set on the individual attending, not the provider or the process.
With little to judge the success of a treatment stay, how can an insurance provider assess whether to continue with a treatment provider? When many individuals return to treatment multiple times ( 3 treatment attempts is an average), are health insurers rewarding mediocrity or even failure to provide effective addiction treatment?
The Florida Model Becomes a Shuffle, California’s Rehab Riviera, and Liquid Gold
Fraud is an almost foregone conclusion when money is readily available and people are unsure of what they are paying for. The floodgates opened for the addiction treatment industry with mandatory health insurance coverage through PPACA and MHPAEA (Seville,2017). Venture capitalists with no addiction treatment experience but plenty of capital funding wanted in on the payday. They just saw an opportunity and banked on it, offering good to mediocre services.
By far the worst was yet to come, as all manner of frauds, schemes, and patient brokering playing on the desperation and misery of so many looking for help. Con artists and nefarious types saw opportunities when a largely unregulated industry with little accountability was given carte blanche to increase treatment access. Soon Florida (Florida Shuffle, 2018), Arizona (Segal, 2017), and Southern California (Rehab Riviera)(Sforza et al., 2017) became epicenters of disreputable sober treatment centers, rehabs, and sober homes.
These areas were by no means the only ones harboring shady operators but their warm climates beckoned to form communities of addiction treatment providers instantly. Literally anyone could open up a rehab or sober home – and they did (Segal, 2017). Even those with previous criminal records and no professional treatment experience, except perhaps their personal substance use, were owners of rehabs, treatment centers, and sober homes. Blocks full of them sprang up seemingly overnight.
What these “entrepreneurs” lacked in treatment experience, they made up for in ingenious ways to scam money from insurance. Set loose with an unlimited “credit card” of insurance coverage, they recruited current or former patients to bring in new patients off the streets, at bus stations, at AA/NA meetings, anywhere they could find them (Segal, 2017). If the new patient had insurance, it was time to put them through the mill of detox-rehab-sober house and back through again as many times as insurance would pay. If the new patient lacked insurance, that was no obstacle. The cost of a monthly insurance premium paid for a new patient to be covered was peanuts to spend for these “treatment providers” compared to the thousands of dollars in insurance reimbursements available to bill on that newly health insurance covered patient.
As if all this weren’t enough, many of these addiction treatment providers decided to bring in extra cash with unnecessary urine screening (Segal, 2017). Urine drug testing is a valuable tool and is a covered service under insurance. Primary and confirmation urine screenings can help track the progress of a patient and may even be mandated by legal systems as part of tangible proof of adherence to sobriety and program attendance. Some of the biggest offenders were using cheap drug tests and billing at exhorbitant rates multiple times for no reason. This “liquid gold” became another avenue to bring in tens, if not hundreds, of thousands of dollars per patient.
If the substance user seemed to move away from using substances, they were tempted with drugs, often by the very people paid to help them. If they didn’t succumb to temptation, they would be put out on the street until they tested “dirty” again and the billing cycle renewed.
Many of these young patients were lured by patient brokers to travel far from home with the promise of luxury beachfront accommodations during their addiction treatment stay. Being away from home produced two desirable points for the treatment providers: a lack of support and oversight from family and friends and the substance user alone in unfamiliar settings with few resources but to agree to play the treatment game. Trusting parents and vulnerable substance users, perhaps already estranged from the chaos of addiction history between them or used to a lack of communication during previous treatment stays, didn’t have a chance to share the deplorable conditions of their stay and the lack of reputable help. This state of noncommunication led for some to disasterous ends as loved ones overdosed in rehabs, in sober homes, on streets, or on the beach. Morgues in Southern Florida (Clary, 2017) continue to be overwhelmed and some families are left with merely the portion of the bill insurance didn’t cover and no loved one to return home.
As an industry, addiction treatment has been plagued with bad actors for decades. Without excusing their actions in any way, these people are taking advantage of a terminally flawed system. When the standard results immediately after leaving treatment are escalation of the type, frequency, or intensity of substance use, and an increased risk of overdose, it’s clear treatment isn’t improving the situation but is actually worsening the outcomes. When the top predictor of relapse after treatment is the strong belief in treatment principles, there is a critical problem. As a nation, we can’t afford to go on this way.
Where Do We Go From Here
It’s said the road to Hell is paved with good intentions and it seems another curbstone was laid with the unfettered access to addiction treatment. No one argues that there shouldn’t be help available for substance users. In the wake of synthetic opioids and analogs, even a one time trial use can prove fatal if someone receives carfentanil or any one of a number of highly dangerous substances mixed in. Deaths are mounting and there is no end in sight.
We are at a critical time. Drug use has been a part of the human experience since the beginning and will remain so. Humans seek novel experiences to enrich their lives, some of these involve chemical enhancement. The fear mongering and substance shaming tactics of treatment don’t work and never have. People successfully quit or moderate their use because it is truly what they want to do.
Decades of research prove that treatment is one of the least effective ways to provide help to a substance user. Ignorance of how to help with addiction isn’t the problem. Providing a level playing field of opportunity for effective substance use alternatives is the challenge. The behemoth of treatment currently controls the conversation and stands to lose a great deal if effective, efficient alternatives are covered by insurance.
Treatment is well aware of this issue. Over time, they have tried to co-op or incorporate some of the best practices and philosophies of alternative programs, but only as overlays or adjuncts to treatment, not a freestanding alternative. The resulting patchwork of adulterated ideas mated to treatment failed and no wonder as many alternative approaches were at cross purposes with the philosophies of treatment. It merely served to confuse the issues further.
Much of that insistence on maintaining treatment fundamentals, despite their continued failure to produce long-term results, has to do with the insurance driven coverage mandates of clinical and medical services, including the need to code addiction as a disease. They need to follow the insurance system to get paid and if they have to force a square peg in a round hole, so be it.
The answer is expanding the conversation and ultimately insurance coverage, to allow effective alternatives equal room on the field without sacrificing the integrity of their approaches to meet a broken and flawed system of reimbursement. We know behavioral health and addiction needs are not being served under the current system. Reforms are inevitable and are, in fact, a golden opportunity for providers and insurance.
Insurance has been the whipping boy of the public and politicians alike. They are an easy target. It doesn’t have to continue but there is a brave new path to forge. An insurance company with the courage to even the playing field for alternative programs to be covered stands to gain cheaper, more effective outcomes for enrollees with lowered repeat treatment costs and increased public good will.
This change to allow access would require front end work to construct alternative measures of service provision but reform is an unquestioned need already for behavioral health and addiction help coverage.
More enrollees survive and do so with fewer or no ongoing medical treatment needs for injuries of substance use. More enrollees return to their lives and careers healthier and able to engage in years of paid premiums with lowered heathcare costs paid out when substance use is lowered or eliminated from their lives. More enrollees seek out addiction help and attendant medical services fewer times over their lives. The human savings are actually profitable.
The market for addiction help actually shrinks, instead of expanding, when alternative approaches that solve addiction rather than promote the never-ending cycles of relapse and recovery are given a fair chance to participate with treatment in insurance reimbursement. Finally, the market self corrects to find the cheapest, effective alternative approaches instead of continuing to subsidize treatment failure.
Billions of dollars and millions of lives hang in the balance of these decisions. Do we continue to push the treatment cart with square wheels down the rutted road of recovery and relapse or is it time to rethink the system of insurance reimbursement with room for approaches that provides for addiction help with efficiency, long–term effectiveness, and profits while saving lives. Make no mistake – change is coming. The potential current and future gains are enormous in terms of lives saved, quality of life preserved, and insurance claim payments eliminated or reduced. Can we afford not to change? What will the choice be?
We Are Ready to Talk – Are You? 888.424.2626
REFERENCES:
American Society of Addiction Medicine. (n.d.). Retrieved April 05, 2018, from https://www.asam.org/resources/the-asam-criteria
Baldwin Research Institute. (n.d.). The Uncertain Present and Future of Addiction Treatment and Insurance Coverage under Mental Health Parity and Addiction Equity Act (MHPAEA) and Affordable Care Act (ACA). Retrieved April 05, 2018, from http://www.baldwinresearch.com/addiction-treatment-insurance-coverage.cfm
Clary, M. (2017, August 28). Rising OD deaths create backlog in South Florida morgues. Retrieved April 05, 2018, from http://www.sun-sentinel.com/local/broward/fl-reg-drug-deaths-rising-20170824-story.html
French, M. T., Popovici, I., & Tapsell, L. (2008). The economic costs of substance abuse treatment: Updated estimates and cost bands for program assessment and reimbursement. Journal of Substance Abuse Treatment,35(4), 462-469. doi:10.1016/j.jsat.2007.12.008
HIV/AIDS. (2017, March 08). Retrieved April 05, 2018, from https://www.cdc.gov/hiv/programresources/guidance/costeffectiveness/index.html
O. (2014, March 04). How Obamacare Is Changing Addiction Treatment Coverage. Retrieved April 05, 2018, from https://www.huffingtonpost.com/2014/03/04/obamacare-addiction-treatment-coverage-aca_n_4896388.html
How The Government Wastes 1.4 Billion Dollars Per Year on Addiction Treatment Research. (n.d.). Retrieved April 05, 2018, from http://www.soberforever.net/addictionblog/index.php/how-to-waste-1-6-billion-dollars-a-year
Implementation of MHPAEA. (2014, August 08). Retrieved April 05, 2018, from https://www.samhsa.gov/health-financing/implementation-mental-health-parity-addiction-equity-act
Jiang, R., Lee, I., Lee, T. A., & Pickard, A. S. (2017, May 30). The societal cost of heroin use disorder in the United States. Retrieved April 05, 2018, from http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0177323
Kirkner, R. M. (2018, January 30). Parity Could Use Some Fixing, But at Least It Won’t Be Dismantled. Retrieved April 05, 2018, from https://www.managedcaremag.com/archives/2018/1/parity-could-use-some-fixing-least-it-won-t-be-dismantled
Mccollister, K. E., French, M. T., Pyne, J. M., Booth, B., Rapp, R., & Carr, C. (2009). The cost of treating addiction from the clients perspective: Results from a multi-modality application of the Client DATCAP. Drug and Alcohol Dependence,104(3), 241-248. doi:10.1016/j.drugalcdep.2009.05.014
Rapaport, L. (2017, August 16). Opioid overdoses leading to more ICU admissions and deaths. Retrieved April 05, 2018, from https://www.reuters.com/article/us-health-overdose-trend/opioid-overdoses-leading-to-more-icu-admissions-and-deaths-idUSKCN1AW2KA
Segal, D. (2017, December 27). City of Addict Entrepreneurs. Retrieved April 05, 2018, from https://www.nytimes.com/interactive/2017/12/27/business/new-drug-rehabs.html
Segal, D. (2017, December 27). In Pursuit of Liquid Gold. Retrieved April 05, 2018, from https://www.nytimes.com/interactive/2017/12/27/business/urine-test-cost.html
Seville, L. R., Schecter, A. R., & Rappleye, H. (2017, June 26). Florida’s Billion-Dollar Drug Treatment Industry Is Plagued by Overdoses, Fraud. Retrieved April 05, 2018, from https://www.nbcnews.com/feature/megyn-kelly/florida-s-billion-dollar-drug-treatment-industry-plagued-overdoses-fraud-n773376
Sforza, T., Saavedra, T., Schwebke, S., Basheda, L., Schauer, M., Gritchen, J., & Wheeler, I. (2017, May 30). How some Southern California drug rehab centers exploit addiction. Retrieved April 05, 2018, from https://www.ocregister.com/2017/05/21/how-some-southern-california-drug-rehab-centers-exploit-addiction/
Statistics. (n.d.). Retrieved April 05, 2018, from https://pharm.ucsf.edu/kidney/need/statistics The economic impact of illicit drug use on American society. (2011). Johnstown, PA: U.S. Department of Justice, National Drug Intelligence Center.
Stevens, J. P., Wall, M. J., Hsu, D., Marshall, J., & Howell, M. D. (2016). The Critical Care Crisis of Opioid Overdoses in the US. American Journal of Critical and Respiratory Care. Retrieved April 5, 2018, from https://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2016.193.1_MeetingAbstracts.A6146.
The Florida Shuffle: The Sometimes Dirty Business of Rehab. (2018, April 05). Retrieved April 05, 2018, from https://www.nbcnews.com/megyn-kelly/video/the-florida-shuffle-the-sometimes-dirty-business-of-rehab-975928899556
The number of daily opioid overdoses in South Florida is overwhelming police. (n.d.). Retrieved April 05, 2018, from https://www.pri.org/stories/2017-04-20/number-daily-opioid-overdoses-south-florida-overwhelming-police
Thielking, M. (2017, December 21). Life Expectancy in the U.S. Is Falling–and Drug Overdose Deaths Are Soaring. Retrieved April 05, 2018, from https://www.scientificamerican.com/article/life-expectancy-in-the-u-s-is-falling-and-drug-overdose-deaths-are-soaring/
Trautmann, S., Rehm, J., & Wittchen, H. (2016, August 04). The economic costs of mental disorders. Retrieved April 05, 2018, from https://onlinelibrary.wiley.com/doi/full/10.15252/embr.201642951
U.S. Department of Health and Human Services (HHS), Office of the Surgeon General, Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. Washington, DC: HHS, November 2016.
Yohanan, M., MD, MPH. (2017). Mental Health Parity: Where Have We Come From? Where Are We Now?(pp. 1-9, Rep.). Seattle, WA: MCG /Hearst Health Network. doi:https://www.ahip.org/wp-content/uploads/2017/06/MCG-White-Paper-Mental-Health-Parity.pdf
DO YOU NEED HELP?
Call Today to learn how the Freedom Model can set you FREE from addiction, treatment, and recovery